Placebos may contain no active ingredients, but they have real effects on the human brain. This article is based on a presentation to the NZ Skeptics 2008 conference in Hamilton, September 26-28.
Earlier this year, Dr Tipu Aamir of the Auckland Pain Management Service drew my attention to something peculiar. In a double-blind, randomised, placebo-controlled trial of morphine after a standard knee operation, 30 percent of those receiving a placebo get pain relief. When those people are given a specific morphine antagonist (‘antidote’), their pain comes back! In the words of a former contributor at an annual conference of this society, this was an epiphany. I needed to know more.
After all, how could something that was ‘all in the mind’ be changed predictably by a substance with a known pharmacological action?
Any study of homeopathy raises the issue of the placebo effect. As a result of a meta-analysis in 2005 of a number of studies comparing homeopathic remedies with orthodox treatment, Shang et al stated in their conclusion that the effect of homeopathic remedies was no greater than that of a placebo. Not that they had no effect, but it was no greater than that of a placebo.
We skeptics are often happy to accept the explanation that if a response to some arcane practice is a placebo response, that settles the issue.
Over the last 30 years there has been a large amount of research into the undoubted effects of placebos. I thought it might be of interest to review this work in the context of our frequent use of ‘placebo effect’ to explain the unscientific.
Placebo is a Latin word for “I shall be pleasing, or acceptable”. It is the first word of the first antiphon of the Roman Rite of the Vespers for the Dead (!), Placebo Domino, dating from the seventh to ninth centuries. Chaucer called one of his characters Placebo in the Merchant’s Tale, because the word had come to mean a flatterer, a sycophant, or a parasite, by the 14th century.
“Placebo seyde: Ful little need had ye, my lord so deare, Council to ask, of any that are here But that ye be so ful of sapience.”
He also uses it in the Parson’s tale: “Flatterers be the Devil’s chaplains, which sing ever ‘Placebo’.”
In the 1811 edition of Hooper’s Medical Dictionary, placebo was defined as “an epithet for any medicine adopted more to please than benefit the patient”. In a recent edition of Collins’ Concise Dictionary of the English Language it is defined as “an inactive substance administered to a patient to compare its effects with those of a real drug, but sometimes for the psychological benefit of the patient through his believing he is receiving treatment”.
However, placebos do benefit patients, and they are certainly not inactive in the context in which they are given.
The most dramatic example of this that I saw in clinical practice involved a young man on artificial kidney treatment. When erythropoietin became available for the treatment of the severe anaemia seen so often in this situation, he was the first patient in our unit to receive it. Erythropoietin is a hormone made in the healthy kidney, which increases the number of red cells in the blood and the amount of the oxygen-carrying haemoglobin. The synthetic version has achieved notoriety as a performance enhancer in sport, for example in the Tour de France. We were all very enthusiastic about this improvement in management for our patient, and he was given his first dose with much interest from all of us. That night he went home, recovered his bicycle from the shed where it had been undisturbed for many months, and rode all around his town with great energy and pleasure. He hadn’t heard the information that the drug took three weeks to act on the anaemia.
We are left with some questions. What was the physiology of his sudden ability to exercise at a ‘normal’ rate, long before there was any change in his blood count? What does ‘it’s all in the mind’ mean? Was he somehow at fault, or was it me and the staff who were lacking in understanding?
I would like to consider:
- The psychological processes involved in the placebo effect
- The physiological mechanisms in the brain
- The site of this activity in the brain
- Why there is variation in the placebo effect from individual to individual
- What are the implications for the classical drug trial format?
Psychological mechanisms
Those who study the psychological processes of the placebo effect cite two major mechanisms.
Conditioning. Pavlov (1849-1936) showed that dogs given meals as a bell rang would subsequently salivate when the bell rang despite not being given food. This process has been explored in humans, who will experience pain relief when a placebo is substituted for a pain reliever when a sequence of active analgesia has been associated with an environmental cue. It is an unconscious process. At the nerve cell level, conditioning leads to a stronger and more sustained response.
Expectancy. This effect is seen when the patient has ‘great expectations’ of the substance being given. These are raised by the conscious or unconscious attitude of the therapist. It is a conscious process on the part of the patient.
It is currently suggested that both conditioning and expectancy are active in the placebo effect, and that in fact, as an inert placebo can have no effect per se, what we see is the effect of the context in which the treatment is given.
Neurophysiology of placebo pain relief
Over the last 30 years, there has been much interest in the neuro-physiological mechanisms of the placebo response.
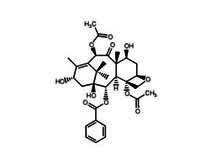
In 1975, Hughes et al identified in the brain two related pentapeptides (a chain of five amino acids linked together) with potent opium-like action. There are many more now identified. These compounds act on specific receptors on the membranes of neurones, and via intracellular metabolic changes increase synaptic transmission. They are made in the pituitary and hypothalamus, and are called endorphins.
A digression
In pharmacology the term agonist denotes a drug with an effect, and antagonist, a drug which specifically blocks the effect of the first substance.
When I spent a year in the pharmacology lab in Dunedin (1959) it was becoming recognised that drugs exerted their effects by way of a specific receptor molecule at the cell surface. The actions of adrenaline, for example, were explained by the presence of two different molecules to which it could attach, which mediated different effects. Noradrenaline would latch on to only one, explaining its more limited range of action. With their usual desire for learned coherency, pharmacologists called them alpha and beta receptors. Antagonist molecules attach to the receptor molecule and block access by the agonist. Hence the term ‘beta-blockers’. These are substances which block the action of adrenaline on its beta receptor. They are widely known for their action in the control of blood pressure, and recently for their unwanted effects when given to protect patients at risk of heart trouble when undergoing operations.
Agonists and antagonists are related by similarities in molecular size, shape, and charge.
Morphine antagonists have been available for some time. In 1961 as a house surgeon in casualty, I was asked to manage an opium addict, brought in because he was deeply unconscious, and breathing perhaps once a minute. He had been without the drug for some weeks, due to market fluctuations. When access was resumed, he used a dose which was the same as his habituated dose. This was much more than he could now tolerate. I had access to nalorphine, a specific morphine antagonist, and 30 seconds after an IV injection, the patient took several deep breaths, sat up, expressed considerable surprise at his surroundings, and then lapsed back into his former state. I was able to repeat this dramatic procedure several times until he recovered!
In 1978 a group of dental surgeons working in California (Levine et al) carried out the following experiment. Patients who had had an impacted wisdom tooth extracted were treated routinely with nitrous oxide, diazepam and a local anaesthetic. At three hours after the procedure they were given either a placebo or naloxone, a specific morphine antagonist. At four hours they were given a placebo or naloxone. Those who had initial pain relief with the first dose of placebo (39 percent), when given naloxone had an increase in pain.
The authors concluded that “this was consistent with the hypothesis that endorphin release mediates placebo analgesia in dental postoperative pain.”
The elegance of this study lies in the unequivocal evidence that a supposedly psychological state (placebo analgesia) was reversed by a specific opioid antagonist. Note that none of the patients was given morphine. There must be a physiological cause for placebo analgesia.
This sort of study has been repeated many times, and always naloxone reverses placebo analgesia.
The site of action of opioids in the brain
The site of this process has been determined. The sites for opioid receptors in the brain can be found by specific cell staining methods and histology on brain tissue. But more exact, ‘real-time’ evidence comes from positron emission tomography (PET) scans.
Another digression
PET utilises short half-life radioactive elements which undergo spontaneous beta decay. In the process, they emit a positron, which collides with an adjacent electron resulting in mutual annihilation, and the generation of two high-energy photons at a near-180 degree angle. These can be detected, and with many, many such events, used to build up a tomographic picture of the source in relation to surrounding tissue. In the studies of the brain, radioactively-labelled glucose is injected, and congregates where activity (utilisation) is greatest. PET scans are used to monitor metabolic activity in specific organs. For example, the extent of heart muscle damage after a heart attack.
In 2002, Petrovic et al were able to show that both opioid and placebo analgesia are associated with increased brain activity in specific regions: the anterior cingulate cortex and the brain stem. There was no increase of activity in these regions with pain only.
Similar localised brain activity has been shown in placebo responses in Parkinsonism (dopamine) and some depressive states (serotonin).
I find these studies exciting and provocative.
Genetic predilection
A further question can be asked in the light of the evidence for a physiological mechanism for the placebo effect. Why does it occur in only 30-40 percent of us for a given situation? It may occur in a greater proportion of a population sample if the context is made more convincing. But why don’t we all have the benefits? Variation in a physiological function begs the question of a genetic predilection.
De Pascalis et al (2002) have shown that individual differences in suggestibility contribute significantly to the magnitude of placebo analgesia. The higher the suggestibility score (there are several tests available) the greater the placebo analgesic effect.
As early as 1970, Morgan et al showed that there was a correlation of suggestibility between monozygotic twins but not dizygotic (fraternal) twins. (Monozygotic twins are the result of the fertilisation of one ovum by one sperm. The resulting zygote splits into two cells which each develop into an individual. These individuals have exactly the same genes.)
Wallace and Persanyi (1989) looked at hypnotic susceptibility and familial handedness. Subjects with close left-handed relatives scored lower in a test for hypnotic susceptibility.
At the 2008 conference, I carried out an experiment with a group of clearly non-suggestible Skeptics. I asked those in the audience to raise their hands if they, or a close relative, were left-handed. If the hypothesis was correct, more than 10 percent of our attendees should have been left-handed. In the event, 22 of 84 attendees indicated they or a close relative were left-handed.
The control study should be done with a church congregation, Protestant or Catholic. In fact, we could do this on both and answer the question as to which is the less suggestible! I haven’t had the nerve to ask. Thomas Bouchard, beginning in 1979, has carried out a number of studies on twins who for a variety of reasons were reared apart. He compared correlations between identical twins and between fraternal twins. The studies from his group (in Minnesota) have shown a large group of correlations in identical twins reared apart, which do not occur in fraternal twins reared apart. The correlations differ very significantly. Table 1 has some examples in twins reared apart:
Similar studies have given similar results in Australia and Western Europe.
Because the nurture of these twins is different, and identical twins have identical genes, the similarities must be genetic. This approach to behaviour has lead to the science of behaviour genetics. (Physical attributes are of course also correlated more between identical twins reared apart, than fraternal twins reared apart.)
Amir Raz (2005, 2008) and his group in New York State have shown that a genetic polymorphism (more than one version of a specific gene) exists for a gene on chromosome 22, which codes for an enzyme active in the breakdown of dopamine, a neurotransmitter. One amino acid substitution (valine for methionine) in the gene alters the enzyme activity by a factor of four times. Since we have a copy of this gene from each parent, we may have val/val, or val/meth, or meth/meth genotypes.
Val/meth heterozygote confers the greater suggestibility. The enzyme is called COMT or catechol-o-methyl transferase.
Brain pathways in which opioid receptors are active are linked to those in which dopamine is the transmitter (nerve to nerve). If there is genetically conferred variation in dopamine activity it is likely that this will influence the result of changes in activity in the opioid pathways.
We must remember that we are talking of a genetic predisposition to be suggestible, and not a gene for suggestibility. It is not that 69 percent of identical twins vote Republican, but that if one does there is a 69 percent probability that the other one does too.
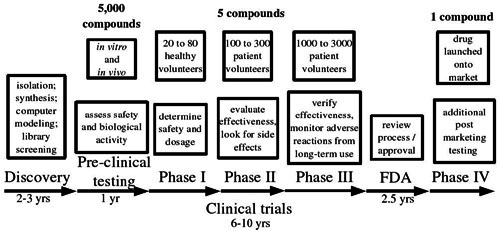
The implications for drug trials
In 2003, Benedetti and his colleagues in Turin examined pain relief in patients after thoracotomy. Patients were allocated to either open infusions of morphine, with information about the efficacy of the drug, or to receive hidden doses of morphine by infusion without any information and without any doctor or nurse present (the open / hidden model for drug trials).
With the same dose, same infusion rate, same timing and same drug, pain relief was less in the ‘hidden’ group.
In the ‘open’ group, the ‘meaning-induced’ expectations had enhanced the drug effect.
This research group has gone on to postulate that in all drug treatment the effect is the sum of actual physiological effect and the effect of expectations. This means that the placebo effect will always cause part of the usual ‘physiological’ response to active drugs. They say that the classical double blind randomised placebo-controlled trial does not allow for expectation effects, and may suggest that a drug has a specific effect gre’open/hidden paradigm’ will give more meaningful results.
Conclusions
- The analgesic placebo effect is accompanied by a distinct, observable, and locatable physiological event in the brain.
- Susceptibility to the placebo effect varies in the population at large.
- This susceptibility is at least in part genetically determined.
- It may be possible to harness this facet of human behaviour for the benefit of individuals, and to prevent its on-going exploitation by charlatans.
- Although placebos are inert and cannot have any effect on the healing processes, their meaning and the context in which they are given can.
- All drug effects include some placebo effect, except when the drug is given surreptitiously. This should alter the classic clinical trial structure.
We have come a long way from the Vespers for the Dead!
Placebos are inert substances but the context in which they are given can alter neurophysiology in such a way as to cause subjective and objective effects.
This is not due to the ‘molecular memory’ of water, nor to strange force-fields as yet unknown to physicists. It is due to our human nature, how we react to our environment, and the relationship, between our minds and our bodies.
Full references available from the editor.